What is CLL?
Leukemia is a cancer of the blood and bone marrow. Bone marrow is the spongy, soft center of bones where stem cells are formed. Stem cells are able to develop into any kind of cell in your body. Some stem cells grow to become blast cells which mature to form different types of blood cells:
- Red Blood Cells – These cells carry oxygen from your lungs to all parts of your body.
- Platelets – These cells help the body form clots to prevent and stop bleeding.
- White Blood Cells – These cells help the body fight germs and prevent infection.
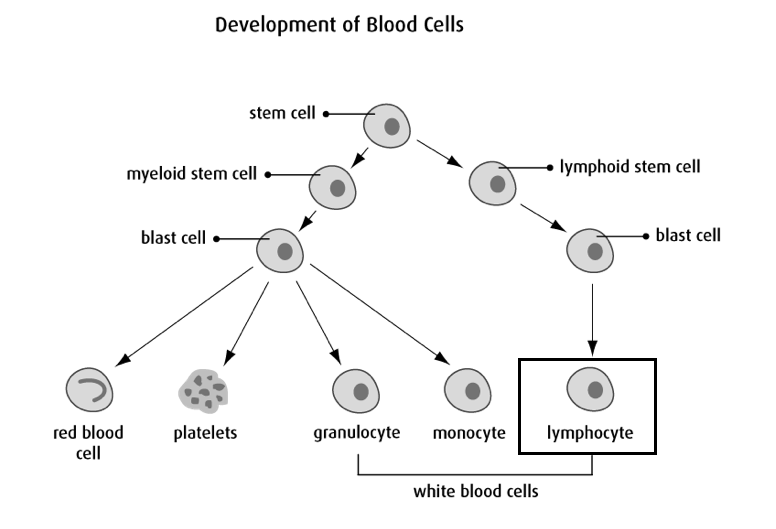
Cancer is the uncontrolled growth of cells in your body. Chronic Lymphocytic Leukemia (CLL) is a slow-growing uncontrolled production of the lymphocyte, which is a type of white blood cell found in your bone marrow, blood, lymph nodes and spleen. Individuals with CLL can often be asymptomatic (have no symptoms) and require no treatment. Others may experience symptoms due to the high lymphocyte levels and the side effects of these high levels. Treatment may be necessary if the patient is experiencing symptoms and/or if the blood cell levels are abnormal.
Symptoms
Anemia is a condition in which you don’t have enough healthy red blood cells to carry adequate oxygen to the body’s tissues. If you have anemia, you may feel very tired, dizzy or short of breath. You may have pale skin and feel weak or cold. There are many forms of anemia, each with its own cause.
In patients with CLL, anemia can occur due to the high level of cancerous lymphocytes overwhelming the bone marrow and causing a decrease in the production of red blood cells.
Patients with CLL can also experience a type of anemia called autoimmune anemia. This is when your own immune system destroys the red blood cells in your body. Because CLL is a cancer involving the lymphocyte, a cell of the immune system, the cancerous lymphocytes can malfunction and attack their own red blood cells.
When a patient experiences anemia, the healthcare team performs blood tests and monitors symptoms to determine the need for treatment and the appropriate management plan.
Thrombocytopenia is a condition in which you have abnormally low levels of platelets in your blood. Platelets are cells that help the blood to clot. Having low platelets can put an individual at increased risk of bleeding and bruising.
In patients with CLL, thrombocytopenia occurs due to the high level of cancerous lymphocytes in the bone marrow causing a reduction in the production of platelets.
When a patient experiences low platelets, the healthcare team performs blood tests and monitors symptoms to determine the need for treatment and the appropriate management plan.
With CLL, the lymphocytes are uncontrollably producing, though at a slower rate compared to acute leukemias. These slow-growing cancerous lymphocytes often reside in areas such as the spleen and the liver. Because of this, the organs can become enlarged and depending on the severity, may or may not cause symptoms. The most common symptom of an enlarged liver and/or spleen is abdominal discomfort. Since the spleen is found on the left side of the abdomen, pain is often localized to the left side, and with the liver located on the right side, pain is often felt in the right abdomen. The enlarged organs can also present as a feeling of fullness, which can cause a decreased appetite and weight loss.
If a patient has an enlarged liver and/or spleen AND is experiencing symptoms because of this, they will likely receive treatment for their CLL.
As with the liver and spleen, the lymph nodes are a common location for lymphocytes to reside. Because of this, the lymph nodes can become enlarged or swollen and though they are usually not painful, some patients may experience some discomfort. Most common locations of swollen lymph nodes include: neck, under the arms (armpits) or in the groin.
Fatigue is a feeling of being very tired. It may not get better with rest or sleep. It is the most common symptom felt by people with cancer. These symptoms are caused by many factors such as low blood counts, infections, eating less food and being less active.
Fatigue can make you feel:
- very tired, weak, worn out, heavy or slow
- like you can’t think or remember things
- like you don’t have the energy to see people or do activities
White blood cells, including lymphocytes, make up an individual’s immune system. Normally, these cells protect you from bacteria, viruses and other harmful organisms you encounter every day. However, individual’s with CLL do not have properly working lymphocytes and therefore experience a weakened immune system, making them more at risk for infections from harmful organisms.
Having a fever is a common side effect of an infection. It is an important signal to tell you that your body may be fighting an infection.
Call or seek medical attention if you have any signs of an infection including:
- A fever. This is a temperature of 38°C (100°F) or higher
- Chills or shaking
- Burning or pain when you urinate
Diagnosis
The diagnosis of CLL is most commonly based on the analysis of a patient’s blood through a blood sample and a physical exam.
Some other diagnostic tests may be required to help come to a definitive diagnosis, such as an ultrasound or CT scan, lymph node biopsy or bone marrow biopsy. These are the most common diagnostic tests used, however; it is by no means an exhaustive list. Your transplant doctor will discuss the specific diagnostic tests required for your individual needs in detail with you.
Blood Draw
A blood draw is performed so the healthcare team can analyze the type of cells in the blood and the characteristics of those cells to determine a diagnosis of CLL. They may also assess organ functions through a blood sample as well at this time.
Physical Exam
A physical exam is required to assess for liver or spleen enlargement and for any swollen lymph nodes.
Ultrasound or CT scan
An ultrasound or CT scan may be required for confirmation of liver or spleen enlargement if the doctor is uncertain after performing the physical exam.
Lymph Node Biopsy
A lymph node biopsy may also be required for confirmation of lymph node involvement if the physician is uncertain after performing the physical exam.
Bone Marrow Biopsy
A bone marrow biopsy is not commonly required to make a diagnosis of CLL but it can be necessary on rare occasion if the physician is unable to make a definitive diagnosis with the blood work and other tests.
Treatments
Treatment is not recommended for asymptomatic patients; however, treatment is considered for those who develop one or more of the following:
- Anemia (low red blood cells)
- Thrombocytopenia (low platelets)
- Enlarged spleen WITH symptoms
- Enlarged lymph nodes WITH symptoms
- White blood cell count increasing quickly
- Other unexplained symptoms interfering with normal daily activities
Treatment commonly consists of the following classes of medication, given alone or in combination.
Chemotherapy medications are anti-cancer drugs that can be injected into a vein or muscle or taken by mouth, in an attempt to control or kill cancer cells. These drugs enter the bloodstream and spread throughout the body. The chemotherapies that are prescribed have been very carefully planned as part of a protocol just for you. A protocol is a precisely timed and organized approach to the treatment of your disease. Before your treatment begins, your physician will review the risks and benefits with, then ask you to sign an informed consent
Chemotherapy is an important part of your treatment and will consist of one or more different types of medications depending on the type of disease you have. The chemotherapy is given on a special schedule that is thought to be best for killing your cancer cells while minimally harming your body. Your doctor will discuss with you what days you will receive chemotherapy, the type of chemotherapy and how you should expect to feel.
Monoclonal antibodies are man-made versions of antibodies that are designed to attach to the surface of cancer cells, causing the immune system to attack and destroy the cancer cells. These medications are often given in combination with chemotherapy as a treatment for CLL.
Note: We are attempting to provide patients with information on the most common treatment utilized; however, it is ultimately up to the Physician to determine the safest recommended course of action for each individual patient.
A stem cell transplant is very rarely used for the treatment of CLL but those with certain cellular abnormalities or those whose cancer recurs after treatment may be considered for transplant.
If your Transplant Physician has informed you that you are going to receive a stem cell transplant, you can download and reference the module below to obtain more thorough information regarding the allogeneic transplant process.
Side Effects and Complications
Most people find it helpful to have information about side effects so they know what to expect and how to manage them. Although the side effects of treatment can be unpleasant, it is important to know that they are usually temporary. Many of these side effects and complications can be treated with medications and careful monitoring.
Remember that all patients are unique. No two persons will have the same experience with side effects. The degree and intensity of each possible side effect also vary greatly from person to person.
Your BMT healthcare team will work closely with you to minimise any discomfort that you may have as a result of your treatment.
What Are the Common Side Effects?
The most common side effects and management of chemo/radiotherapy are:
Allergic reactions are common with a medication called Rituximab that is can be used for treatment of CLL. Signs of an allergic reaction may include: flushing, rash, hives, itching, dizziness, swelling or difficulty breathing. Allergic reactions commonly occur during or right after receiving the first or second dose of Rituximab.
Be sure tell your nurse if this happens while you are receiving the medication or contact your doctor/seek medical attention if this happens after you have left the unit.
Anemia is a condition in which you don’t have enough healthy red blood cells to carry adequate oxygen to the body’s tissues. Having anemia may make you feel tired and weak. There are many forms of anemia, each with its own cause.
Some treatments can reduce your red blood cells and cause anemia. If you have anemia, you may feel very tired, dizzy or short of breath. You may have pale skin and feel weak or cold. The symptoms will go away as your body produces more red blood cells. We monitor your blood tests to determine if you need blood transfusion.
What can help:
- Tell your health care team if you are feeling dizzy or weak. Depending on what your blood results are, you may receive a blood transfusion.
- Move slowly to avoid getting dizzy. When you get out of bed, sit on the side of the bed for a while before you stand up. Once you stand up, ensure you feel stable on your feet before you start walking.
- If you’re feeling weak or dizzy, call a nurse (or family member when at home) to help you to your chair or the bathroom. This is not an imposition; it is much safer for you to accept help than for you to fall and injure yourself.
- Try to eat foods that are high in iron, such as green, leafy vegetables, liver and cooked red meats. A dietitian can help you choose foods that may help you feel better.
- Limit some of your activities. Do only what you have to or what is most important to you.
Undergoing cancer treatment can affect every part of your life, including your body, feelings, relationships, self-image and sexuality. Some patients say that the emotional impact of treatment can be harder to manage than the physical changes.
Anxiety is feeling afraid, overwhelmed or very worried. Feeling anxious when you have cancer is normal, but if your anxiety becomes worse and starts to take over your thoughts and your daily life, tell your healthcare team. They can recommend someone you can talk to or give you medicine that can help.
Your emotions can change from day to day, or minute to minute. Your emotions may also change depending on there you are at in your treatment process. Some emotions can be caused or made worse by certain chemotherapy drugs as well as some hormonal therapies, steroids and pain medicines.
Some of other feelings you may have include:
- Hopelessness, helplessness, uncertainty, impatience, isolation
- Being out of control and overwhelmed
- Fear of sickness, death or the unknown
All of these feelings are normal, but it is important to tell your healthcare team when you are feeling this way.
What can help:
- Let your health care team know you are feeling anxious. We can listen and help reassure you. Ask us questions so you will know what to expect.
- Write down your thoughts or share your feelings with people you trust.
- Talk to someone who has been through it. Connect with a peer support program, available through community cancer centers.
- Eat well, get enough sleep and stay active. Try to take a 10-15 minute walk each day to boost your mood and energy.
- Distract yourself by focusing on or doing an activity you enjoy. This will give you some relief from your thoughts and feelings. This may include things like: reading, meditation, listening to music, watching a favourite TV show or movie, painting, sketching, knitting, spending time with family and friends, etc.
- Put on headphones, close your eyes, and listen to something that will make you feel relaxed or happy: music, guided meditation, audiobooks, podcasts, etc.
- Look for relaxation and meditation apps for your portable device (i.e. Calm® and Headspace® apps can be trialed for free before purchasing).
- Try relaxation techniques such as deep breathing, meditation, reiki or yoga.
- Set realistic small goals (“Take one day at a time”). When you feel overwhelmed or you think what lays ahead will be too long or tiring, try taking it one day or even one hour at a time. This helps you focus on the here and now and see your progress one step at a time.
- Spend time with people who make you laugh.
While you’re receiving treatment, your body needs more energy than usual. Eating helps you heal. Getting enough calories, proteins, vitamins and minerals will help prevent muscle and weight loss and may also cause less treatment side effects.
You may not feel like eating because of nausea or because of a sore or dry mouth. Appetite loss, fatigue, taste changes, stress or depression can make you want to eat more or less than usual.
What can help:
- Ask your nurse for a referral to one of our dietitians. They can offer helpful suggestions specific to your situation.
- Eat whatever you can manage, even if this means eating the same foods for a while. Your taste sensations will eventually improve.
- Instead of big meals, eat smaller meals and snacks more often.
- Relax and take your time while eating. Eat when your energy is highest.
- Eat what works for you. Eat breakfast foods at suppertime if you feel like it.
- Save your favourite foods for when you are feeling better. Eating your favourite food when nauseated can make you not like them.
- Try to add calories and protein to meals: peanut butter, higher fat milk, cream, eggs, cheese, yogurt, tofu, gravies, ice cream, nuts, beans.
- Higher nutrient fluids: fuller fat milk, smoothies, meal replacement drinks, cream soups, and hot chocolate. (Caution: dairy products can cause diarrhea).
- Light exercise and a walk before meals can help boost your appetite.
- Try the “Mind over Matter” approach. Even though you may not feel like eating or not find it enjoyable, think of food as something your body needs for you to heal, much like a medicine.
- Be patient with yourself, your appetite will come back.
- For help with taste changes, type “Food ideas to cope with taste” on www.bccancer.bc.ca or talk to your dietitian.
The urinary tract is a common area for infection. Patients that receive a medication called cyclophosphamide are also at increased risk of inflammation of the bladder. This can resemble a urinary tract infection with symptoms including burning and frequent urination as well as visible blood or blood clots in the urine. This complication is called hemorrhagic cystitis.
What can help:
- Drinking lots of fluids while you receive cyclophosphamide is recommended in order help flush out the bladder.
- You are also encouraged to urinate as soon as you get the urge in order to prevent the drug from sitting in the bladder for too long.
Some chemotherapy drugs can cause your body to make fewer platelets. Platelets are cells that help the blood to clot. Without enough platelets, you may get bruises even when you haven’t bumped into anything.
We use blood tests to monitor your platelet levels. We generally give you a platelet transfusion when your levels drop below 10-20, if you are bleeding, or before certain procedures.
What can help:
- Talk to your nurse or doctor about any bleeding or bruising issues. Depending on your blood results, we may give you a platelet transfusion.
- Be extra careful to not bruise, cut or burn yourself.
- Blow your nose gently to prevent a nosebleed. Do not pick your nose.
- Use a very soft toothbrush or cotton swabs to clean your teeth.
- Use an electric shaver instead of a razor. Electric shavers are available for use on the inpatient unit, ask your nurse.
- If you are female and are having bleeding or spotting from your period, talk to your nurse or doctor.
- Petechiae (“puh-tee-kee-ah”) are small purple or red spots on your skin that usually appear in clusters. They happen with a lower platelet count and although they are not harmful, they need to be watched.
- Be extra careful when you use a knife, scissors or any sharp tool.
- Call us immediately if you have any of the following:
- Vomit that looks like coffee grounds
- Black, tarry bowel movements
- Bright red blood in your urine or stool
Constipation means you’re not having bowel movements as often as you used to. Your stool becomes hard and dry, and having a bowel movement can be difficult or painful.
Changes in your normal bowel movements may be caused by drug treatments for cancer or other drugs you’re taking to manage nausea, diarrhea, depression, blood pressure changes, or pain. Constipation can also happen because you’ve changed your eating habits, you’re drinking less liquid or you’re less active.
What can help:
- Talk to your nurse, dietitian and doctor. They can help suggest stool softeners, laxatives and other diet options that can help with constipation symptoms.
- Add more fibre to your diet, a little at a time. Examples of foods with high fibre are whole grain breads and cereals, brown rice, vegetables, fruit (including dried fruit), legumes, beans, seeds and nuts.
- Drink plenty of liquids throughout the day. Try water, fruit or vegetable juices, teas and lemonade. Hot or warm liquids like cocoa, tea or lemon water can also help.
- Eat natural laxatives such as prunes, prune juice, coffee, and papaya.
- Be more physically active. Just taking a walk can help.
- Do not strain to have a bowel movement. This can cause issues with bleeding, infection and hemorrhoids. It can even cause you to faint on the toilet.
- Do not use any rectal suppositories or enemas while receiving treatment. They can cause bleeding and increase the risk of infection.
Depression means feeling sad, hopeless, and/or feeling the loss of pleasure in nearly all activities. All of these feelings can come and go. But it could be a sign of clinical depression if:
- the feelings become worse or last a long time
- you also feel worthless or guilty or have regular thoughts of death or suicide
- you also have changes in appetite, weight or sleep or have a hard time thinking
- the feelings start to take over and negatively affect your daily life
Depression can and should be treated. It is not a sign of weakness. A person who is clinically depressed can’t just “cheer up” through will-power alone. There are treatment options available such as counselling and anti-depressant medications.
What to watch for (possible signs of depression):
- feeling hopeless or worthless
- crying a lot
- not sleeping or sleeping too much
- overeating or having no interest in eating
- thoughts of harming yourself
What can help:
- Ask for help. Tell your loved ones and/or your health care team that you’re having trouble.
- Other recommendations can be found under Anxiety and Stress.
Diarrhea means you have soft, loose or watery stools more than 3 times in a day. You may also have cramps and bloating or feel an urgent need to have a bowel movement.
Some drugs can cause diarrhea, but it can also be caused by infections. It’s important to tell your healthcare team if you have diarrhea so we can determine the cause and how we can help you best manage it.
What can help:
- Tell your nurse or doctor if you have diarrhea. Depending on how frequent it is, a sample may be taken to test for infection.
- Use soft toilet paper. Clean your bum with mild soap and water after each episode of diarrhea. Rinse well and pat dry with soft toilet paper.
- Tell your nurse or doctor if you have any pain or bleeding in your rectal area.
- Drink plenty of fluids, at least 8 to 10 large glasses a day. Try water, broth, fruit juices, Jell-O and sport drinks.
- Eat high potassium foods such as bananas, apricots and peach nectars, meats and potatoes.
- Limit the use of irritants such as coffee, chocolate and prune juice.
- Ask your doctor before taking any over-the-counter medications for diarrhea.
- Consider using a sitz bath, a seat that sits on your toilet. This allows you to soak your genitals and rectal area to help clean and relieve pain. Sitz baths are available on the inpatient unit and at any local pharmacy.
- Ask your nurse about the use of protective barrier creams you can use to reduce the amount of skin irritation from frequent wiping.
Fatigue is a feeling of being very tired. It may not get better with rest or sleep. It is the most common symptom felt by people with cancer. These symptoms are caused by many factors such as low blood counts, infections, eating less food and being less active.
Fatigue and malaise can make you feel:
- very tired, weak, worn out, heavy or slow
- like you can’t think or remember things
- like you don’t have the energy to see people or do activities
Fatigue usually goes away over time after cancer treatment ends. For some people, it can take a long time to go away completely.
What can help:
- Tell your healthcare team. It’s possible that you may need medicine, a nutritional supplement or a blood transfusion to help with your symptoms.
- Think about the “4 P’s of Energy Conservation”
- Prioritize: When you have more than one thing to do, begin with the most important task to make sure it gets done.
- Plan: Plan your activities in advance to avoid doing extra trips.
- Pace: Never rush. Rest often and rest before you feel tired.
- Position: Sit when you can to do tasks. Avoid bending and reaching too much.
- Rest when you need to. Take short naps of 10 or 15 minutes rather than longer naps during the day. Too much rest, as well as too little, can make you feel more tired. Save your longest sleep for the night.
- Balance your rest and activity. Keep track of when you feel most tired and when you have more energy so you can plan activities at the best time.
- Try to limit the length of visits with family and friends. In hospital, ask your nurse if you need help limiting the length of time visitors stay.
- Update family and friends with group texts/emails or social media (or delegate this task!).
- Let others help. Ask friends and family to grocery shop, cook, or babysit.
- Drink plenty of fluids, especially water. Frequent smaller meals can be easier than 3 large meals.
- Light exercise such as walking around the block or unit can boost your energy.
- Find support. Talk to someone about how your fatigue makes you feel. Join a support group in person or online.
Fertility problems for a man mean he can’t get a woman pregnant. For a woman, it means she can’t get pregnant or can’t carry a pregnancy to term. Some chemotherapy and radiation treatments can cause temporary fertility problems, and sometimes they can cause permanent fertility problems. Infertility does not affect your ability to have or enjoy sexual intercourse.
Men may be able to have their sperm frozen and saved in a sperm bank before treatment begins; discuss this with your doctor as soon as possible. For newly diagnosed females, we recommend you talk to your doctor but it is usually not possible to arrange for embryo (egg) freezing before starting treatment. This is a lengthy process that can take 2 to 6 weeks and unfortunately, any delay in cancer treatment could be life threatening. It is sometimes possible for females to deliver healthy babies after cancer treatment is complete.
Preventing Pregnancy
Since not all chemotherapy medications can cause infertility, pregnancy may be possible during treatment. However, because chemotherapy damages egg and sperm cells, there could be birth defects or harm to an unborn baby. For that reason, it is important to prevent pregnancy.
If you are sexually active during treatment, please use a form of birth control. Talk with your doctor about birth control options and when it is safe to stop using it.
Coping with Changes in Fertility
Infertility can be very hard to come to terms with. The sense of loss can be strong for women and men of all ages. It can be very difficult to learn that you may no longer be able to have biological children. You also may be very sad or angry that the treatment has caused changes to your body and your self-confidence may be affected. It can help to talk to your partner, a relative or friend about how you are feeling.
More resources can be found at:
www.olivefertility.com/- Clinics in Vancouver, Surrey and North Vancouver. This is where most male patients have sperm banking done.
Some chemotherapy drugs can cause temporary hair loss or thinning. Hair loss usually starts 2 or 3 weeks after treatment begins. It may start gradually or your hair may come out in clumps. Hair loss can happen anywhere on your body.
Hair loss is usually temporary. Your hair may begin to grow back while you’re still having treatment or it may take 3 to 6 months after treatment to start growing back. Some people find that their new hair is curlier or slightly different in colour than before.
What can help:
- Be gentle with your hair. Use a mild shampoo and a soft hairbrush.
- Consider cutting your hair short before it falls out. Longer hair comes out easier and makes hair loss more noticeable. A family member or salon can help you cut or shave your hair, or a nurse can assist you on the inpatient unit. This is your choice and you will know if and when you feel comfortable to do so.
- Use hats, head scarves, or wigs to keep your head warm and protected.
- Protect your scalp from the sun using a hat or scarf and/or sunscreen.
- If you’re interested in a wig, choose one before your hair falls out. You’ll be able to find a close match to your own hair colour and style more easily.
- Ask your insurance company if it will cover the cost of a wig. If not, you can deduct the cost as a medical expense on your income tax return.
- Prepare your family and friends. People close to you, especially young children, may need to be reassured when they see that you are losing your hair.
- Talk about your feelings. Hair loss can sometimes be hard to accept.
The chemotherapy you are given lowers your white blood cells. Normally, your white blood cells protect you from the bacteria, viruses and other harmful organisms you encounter every day. Without your white blood cells, any type of germ can make you sick with an infection.
Having a fever is a common but serious side effect. It is an important signal that tells us your body may be fighting an infection. We act quickly when you have a fever in order to stop an infection from causing serious harm.
Most patients on our units have weak immune systems (low white blood cells). We take extra care to protect everyone through infection prevention.
What can help:
- Take your antibiotics, antifungals and antivirals as instructed. These medications help protect you from infections while your white blood cells are low.
- Proper handwashing is the best way to prevent infections. You and all of your family members and visitors should wash your/their hands often with soap and water, especially before eating and after using the toilet. Carry a bottle of hand sanitizer when you are out of your home.
- Check your temperature twice a day: in the morning and early evening. Check it more often if you’re feeling unwell.
- Do not take Tylenol® (acetaminophen) unless we instruct you to.
- Call us immediately if you have any signs of an infection including:
- A fever. This is a temperature of 38°C (100°F) or higher.
- Chills or shaking
- Burning or pain when you urinate.
- Family and friends should NOT visit you if they have any signs of illness (i.e. new cough, fever, diarrhea, vomiting, sore throat, runny nose, etc.).
- Shower daily or every other day. Keep your body clean.
- Clean your anal area gently but thoroughly after a bowel movement. Wipe from the front (genitals) to the back (rectum) to avoid urinary tract infections.
- Avoid touching your face and mouth with your hands.
- Avoid crowded areas such as malls, markets, buses, and movie theatres.
- Do not go swimming or use hot tubs if you have a CVC IV line or a low white cell count.
How and When to Take Your Temperature:
- Take your temperature with a digital thermometer in Celsius twice a day: when you get up in the morning and in the early evening (around 6pm).
- Take your temperature more often if you don’t feel well.
- Don’t take your temperature after eating or drinking. Wait 5 minutes.
- Clean your thermometer with warm water and dish soap. Allow to air dry.
- Call us immediately if you have a fever of 38°C (100°F) or higher. We will give you instructions to follow.
It can be common to develop a dry or sore mouth several days after chemotherapy. This is referred to as mucositis (“mew-co-SYE-tiss”). You may notice small canker sores on the inside of your cheeks or lips, under your tongue or on the base of your gums.
What can help:
- Tell your nurse or doctor if you have pain or notice sores in your mouth or throat. Special mouth rinses can numb your mouth and throat to make it easier to swallow. Pain medications can also be used for comfort and to help you eat.
- Brush your teeth with a soft toothbrush. You will be prescribed a special mouth rinse to use before breakfast and at bedtime. Add water it if tastes too strong.
- Use lip balm to keep lips moist and prevent cracking.
- It is safe to floss if this is your usual routine but stop if you notice bleeding gums.
- Try soft foods that are moist, bland and easy to chew or swallow such as eggs, smoothies, cream soups, yogurts, cooked cereal, mashed potatoes, ice cream and ground meats. Gravies, sauces and soups can help soften foods.
- Eat whatever you can manage but try to avoid hot, spicy, acidic, hard or crunchy foods such as toast and hard tacos.
- Ice chips, hard candies and popsicles can help relieve dry and sore mouth.
- Remove dentures often to give your gums a rest. Keep dentures clean.
Some drugs can make your muscles feel weak or make you lose your balance. They can affect your nerves, causing numbness or a tingling (pins and needles) or burning feeling in your hands or feet. Usually, these side effects are temporary. But for some people, they may last for several months after treatment is over or may be permanent. Let your healthcare team know if you have any symptoms of weak muscles, numbness, or tingling in your fingers.
What to watch for (signs of muscle or nerve problems):
- tingling, burning, weakness or numbness in your hands or feet
- sensitivity to hot and cold or being less able to feel hot and cold
- pain when walking
- weak, sore, tired or achy muscles
- shaking, trembling, or losing your balance
- increased difficulty doing your day to day tasks (i.e. walking, picking up objects, buttoning your clothes)
Talk to your healthcare team if you have any of these problems.
What can help:
- Be careful with sharp objects so you don’t cut yourself.
- Check the bottom of your feet for cuts or other wounds.
- Move slowly and use handrails when you go up and down stairs.
- Use no-slip mats in the bath and shower; install grab bars.
- In your house, keep all areas clear so you don’t trip.
- Protect your feet with shoes, socks or slippers.
- Use gloves when taking food out of the freezer.
- Test the water temperature with a thermometer before taking a bath.
- Regular exercise and activity can prevent weakness.
Nausea is when you are feeling sick to your stomach and feel like you have to throw up (vomit).
What can help:
- Talk to your nurse, doctor and dietitian.
- Take prescribed anti-nausea pills as instructed and take more “as needed”.
- Instead of big meals, eat smaller meals and snacks more often.
- Avoid foods that are very sweet, greasy, fried or spicy or that have a strong smell.
- After eating, avoid lying down for at least half an hour.
- Relax and take your time while eating.
- Save your favourite foods for when you are feeling better. Eating your favourite food when nauseated can make you not like them.
- Sip water and other liquids (ginger ale, sports drinks, broth) throughout the day.
- If you’re feeling nauseated, take deep slow breaths through your mouth or place a cool cloth over your eyes and forehead.
- Distract yourself by listening to music, watching a movie or talking to loved ones.
- Smelling (not eating) aromatherapy oils can be helpful with nausea.
- Cannabis has anti-nausea effects although its use on hospital property is restricted. For more information, talk to your healthcare team.
Foods and fluids that may be easier to eat:
- Broth, water, peppermint tea, ginger tea
- Popsicles, watered-down juices, Gatorade®, “flat” pops (i.e. ginger ale)
- Jell-O®, sherbet
- Soda crackers, Melba toast, pretzels, dry cereals, dry toast, plain cookies
- Boiled potatoes, noodles, rice, congee
- Light soup – chicken and rice, vegetable
- Boiled or baked lean meat, poultry and fish
- Skim or 1% milk, low fat yogurt, cheese
- Applesauce and fresh, frozen or canned fruit and vegetables
Avoid foods that can make nausea worse:
- Fried meats, fried eggs, sausage, bacon
- Broccoli, brussel sprouts, onion, garlic
- Doughnuts, pastries, coffee, other rich sauces and foods
When Should I take “As Needed” Anti-Nausea Medications?
Your doctor will prescribe you anti-nausea medications to take “as needed.” They can be given in pill or capsule form or, while you’re in hospital, intravenously (IV).
Anti-nausea medicines work best when you take them before or as you’re starting to feel sick. They may not work as well if you take them just as you are about to throw up (vomit). If you’re feeling nauseated and one medication doesn’t work after an hour, try a different one. Tell your doctor or nurse if these medications do not relieve nausea and vomiting. They can make suggestions or prescribe other medicines.
If you have nausea and vomiting at certain times of the day, take or ask for your anti-nausea medicine at least 30 minutes before that time. For example, if you often have nausea or vomit with meals, take an anti-nausea medication at least 30 minutes before your meal. If you vomit within 1 hour of taking your anti-nausea pill, you can take another pill.
Anti-nausea medications can cause side effects, including sleepiness, constipation, or diarrhea. Most people feel that these side effects are worth the benefit of having their nausea relieved.
Pain is more than just hurting. It’s also uncomfortable and upsetting. When you’re in pain, it can be harder to fight cancer or perform day-to-day activities.
What can help:
- Tell your health care team if you are experiencing pain. They can suggest comfort measures and sometimes pain medications that can help your body relax and rest. Your body needs rest and relaxation to be able to heal.
- Discussing what causes your pain, what type of pain it is and its patterns can help you and your health care team prevent or lessen it. For example:
- Where do you feel pain? When did it start? What makes it better or worse?
- What does the pain feel like? Is it dull, sharp, burning, pinching, stabbing?
- How strong is the pain from 0 to 10, (0 is no pain, 10 is worse pain imaginable)
- Try to stop pain before it gets worse: Sometimes people wait until their pain is bad or unbearable before taking medicine. Pain is easier to control when it’s mild. If you wait, your pain can get worse, it may take longer for the pain to get better or go away, or you may need larger doses to bring the pain under control.
- Tell your healthcare team if you have any side effects from your pain medicine. Many people choose not to take or stop taking their medication because of side effects, but they can often be managed.
- Try relaxation techniques. Relaxation can help relieve tension and pain.
- If possible, continue to stay active. Gentle stretching and movement may help.
Side effects of treatment (such as hair loss, hormone changes, fatigue and emotional changes) can affect your sexuality and the way you see yourself. Common sexual changes include body image concerns, low sexual desire, vaginal dryness, difficulties with erections, pain during sexual activity, and relationship changes.
What can help:
- Talk openly about your feelings with your partner. No one can read your mind, not even someone you have lived with for years.
- Being physically active improves self-image and energy.
- There are many ways to express your affection and be intimate with your partner. Touching, holding, cuddling, taking walks, good conversation, hugging, kissing, and dancing are important aspects of intimacy.
- Talk with your health care team if you have questions or concerns about sexual or body changes, birth control, periods (menstruation) or fertility.
It is safe to have sex once your blood cell counts have recovered. Platelets should be higher than 50 and white blood cells should be 1.0 or higher. It’s important to use some sort of birth control to prevent pregnancy while you’re receiving cancer treatment. If a pregnancy happens with an egg or sperm that has been damaged by chemotherapy or radiation, there is an increased risk for birth defects.
Suggestions to make sex more comfortable:
- Wash your hands before and after sex or masturbation.
- Use a water or silicone-based lubrication to help with comfort and dryness. It should be BPA and Phthalate free, the pharmacist at your local pharmacy can help you find a suitable option. If it smells, tastes or tingles, it shouldn’t be used.
- Find positions that are comfortable. Use pillows as extra support.
- Use medical grade silicone or glass vibrators or personal assistive devices. Wash them before and after in hot soapy water. Do not use antibacterial wipes on them.
Some chemotherapy drugs and radiation can cause skin rashes, redness, itching, dryness, peeling or acne-like blemishes. A rash usually starts within a few weeks of starting treatment. It may start as redness or a warm feeling like a sunburn. The colour of your skin may become darker. Some drugs may make your fingernails and toenails become darker, ridged, yellow, brittle or cracked.
These skin conditions usually go away once treatment is over. Your healthcare team can suggest a treatment specific to your symptoms (i.e. creams, or antihistamines – Benadryl® – to reduce itchiness.)
What may help:
- Tell and show your health care team any skin changes right away.
- Wash with a gentle soap to reduce your risk of skin irritation and infections. Wear loose, comfortable clothes.
- In the shower, use warm water instead of hot. Gently pat your skin dry rather than rubbing it.
- Use a gentle moisturizer to soften your skin and help it heal if it becomes dry or cracked.
- If your skin feels itchy or irritated, try gentle massage or pressure on the area. You can also apply a cool, damp cloth to itchy areas.
- Keep your nails short and clean. Use cuticle cream instead of cutting the cuticles.
- If you cut or scrape your skin, clean the area at once with warm water and soap.
- Petechiae (“puh-tee-KEE-ah”) are small purple or red spots on your skin that happen with a lower platelet count. They are not harmful but need to be watched.
- Your skin will become more sensitive so you should protect your skin from the sun by wearing a wide-brimmed hat and clothing that covers your arms and legs. Apply sunscreen with a SPF of at least 30 when you go outside, even if it is cloudy.
- Avoid hot water bottles and heating pads, they can seriously burn your skin.
Having trouble sleeping (insomnia) is a common problem during treatment. You may have insomnia if you are unable to fall asleep, wake up often during the night or wake up very early and can’t go back to sleep.
Pain, anxiety, depression and some medicines can affect your sleep. Insomnia makes it harder to cope with other side effects of treatment. It can affect your mood and energy level, cause fatigue and make it hard to think and concentrate.
What can help:
- Take only short naps (15-20 minutes) during the day.
- Be as active as you can during the day. This can give you more energy for the day and help you sleep better at night.
- Go to bed and get up at the same time every day.
- Your doctor can give you a sleeping pill to help you sleep, especially on the inpatient unit. Think of this a short-term solution. Do not depend on it to sleep.
- Relax before bedtime – have a warm shower, read, listen to music, audiobooks or podcasts. Avoid looking at the TV, cell phone screens and other electronic devices.
- Do not have caffeine at least 6 hours before bedtime. Caffeine is found in coffee, non-herbal tea, chocolate, and soft drinks. Try not to eat a heavy meal or drink within 2 hours of bedtime.
- Make sure your bed, pillows and sheets are comfortable. Block out distracting light, or use a sleep mask. Ear plugs are available on the inpatient unit.
- Get up and go into another room if you’re tossing and turning in bed. Stay there until you feel sleepy enough to return to bed.
- On the inpatient unit, your occupational therapist (OT) can help with sleeping issues and other strategies to make you more comfortable.



